India’s mental health burden is well documented: one in seven people suffer from mental illness and approximately 70–92 percent of disorders go untreated. According to the World Health Organization, the prevalence of mental health problems in India is estimated to produce economic losses of approximately USD 1.03 trillion between 2012 and 2030. These financial setbacks could result from poor mental health in the workplace, which affects employees’ productivity and performance and increases attrition levels. At the household level, out-of-pocket expenditure on mental healthcare can push an Indian family below the poverty line.
Given the massive scale of the challenge and its implications for the country’s social, economic, health, and sustainable development, government support is critical. However, this alone can’t address the crisis. Over the past five years, public spending on mental health in India has stagnated at approximately 1 percent of the overall health budget, showcasing the necessity of philanthropic and private sector resources in bridging funding gaps.
The flexible nature of philanthropic giving means that it is far better positioned to make a greater impact and create long-lasting change, especially where it is needed the most: at the primary care level. It can also provide risk capital for innovation, science, and research—something that is much needed in the field.
To understand Indian philanthropy’s response to mental health challenges, the Centre for Asian Philanthropy India (CAPI) conducted semi-structured interviews with 43 donors, nonprofit leaders, and experts from 31 organisations working to improve mental health. The insights from these interviews are detailed in a report titled Mindful Investments: Philanthropy for Mental Health in India. The report highlights key approaches to mental health in Indian philanthropy, challenges in the funding landscape, and recommendations and opportunities to help donors better address India’s mental health needs.
Here are some of its key findings.
Philanthropic funding for mental health is limited but is on the rise
India is still a low-income economy with numerous competing needs for resources across nutrition, education, housing, and physical health. Consequently, much philanthropic giving ends up focusing on these causes. Physical health and education, for instance, made up 55 percent of philanthropic contributions as of 2023.
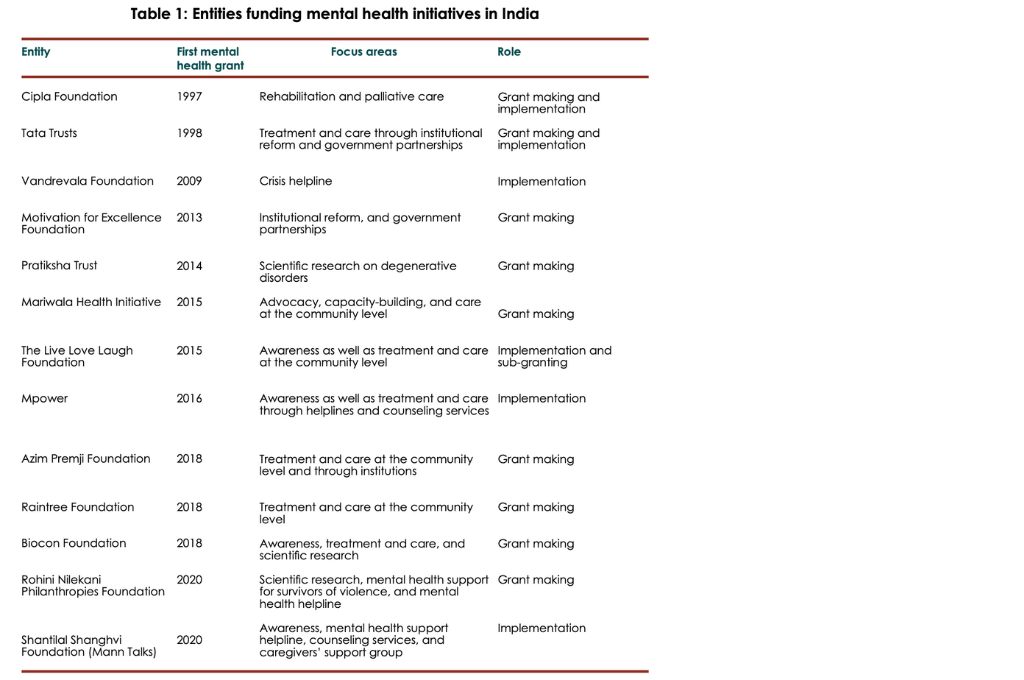
Given this, mental health has been a low priority for donors in India. However, in the last decade or so, domestic giving for mental health programming has seen a shift. The shared experience of the pandemic and the subsequent rise in awareness and sensitisation around mental illness have helped turn donor attention towards this critical topic. As a result of this, at present, many domestic donors—both individuals and philanthropic foundations—have created a separate portfolio or vertical to fund mental health interventions. Of these, some—such as Vandrevala Foundation, Mariwala Health Initiative (MHI), and The Live Love Laugh Foundation— focus exclusively on mental health. Others, such as Tata Trusts and Azim Premji Foundation, fund or implement mental health initiatives within broader efforts in health or disability and inclusion.
Three key approaches in philanthropic giving
Although in its nascency, mental health philanthropy in India is growing and adapting to address the continuum of needs in this field. We observed three key approaches in how domestic donors currently support mental health. These are not mutually exclusive and some donors adopt a combination of the three.
1. Institutional approach
This approach is adopted by a majority of Indian donors. The strategy here is to provide treatment and care to those suffering from mental illness through institutions or facilities and via qualified medical and paramedical professionals. Donors support such facilities to address immediate needs, because they are particularly helpful for those with severe mental illnesses that require focused care from specialists.
In this context, funding is directed to set up new centres for mental health treatment or enhance existing ones. For example, Udaan, a collaboration that began in 2016 between two donor entities—Tata Trusts and the Government of Maharashtra—was pivotal in reforming the Regional Mental Hospital in Nagpur district. The hospital, established in 1864, underwent significant changes aimed at enhancing its therapeutic environment. This included infrastructural upgrades such as new wards, a library, and a meditation hall. Concurrently, clinical processes were revamped, and the staff participated in upskilling programmes. Udaan also actively focused on creating employment pathways for its patients by setting up a bakery, a mobile cafeteria, a tailoring unit, and agricultural initiatives. Finally, it also emphasised reintegrating patients with families through a mix of halfway homes and individual interventions.
More recently, in September 2023, Cipla tied up with NIMHANS to set up a neuropalliative care unit. Cipla’s ‘family care’ model of palliative services provides patients and their families emotional and psychological support, alongside nutrition, physiotherapy, and pain management and medical care.
Donors also fund or set up helplines to offer remote counselling and assistance in managing emergencies such as suicide prevention. Helplines are relatively easier and quicker to set up, not requiring heavy investments in infrastructure. Many funders gave to helplines during COVID-19, when people could not travel to clinics. For instance, Mann Talks—funded by Shantilal Shanghvi Foundation—was set up during the pandemic as an emergency helpline. Mann Talks has since expanded its services to longer-term programmes such as appointment-based online counselling sessions, and a support programme for caregivers of terminally ill patients.
2. Community-led approach
In the last few years, a few donors have begun funding community-led approaches in order to bring caregiving outside of institutions and directly to individuals in need.
Rather than relying on psychiatrists or psychologists, who are in short supply in India, the community mental health (CMH) model draws resources from the community. Under this model, care is delivered by trained community-based workers such as women-led self-help groups (SHGs), auxiliary nurse midwives (ANMs), accredited social health activists (ASHAs) and other social workers, as well as grassroots volunteers with the recognition that tasks such as basic counselling, raising mental health awareness, and ensuring medication adherence can be carried out by non-specialists. In turn, these community volunteers can and do provide referrals up the value chain for more severe conditions.
India’s historical preference for institutionalised care further hampers funding directed towards community-based approaches.
Some CMH models are broader in design and their scope is not restricted to mental health. Often, these focus on other socio-economic or systemic issues—such as poverty, lack of rural development, or the adverse effects of climate change—that contribute to poor mental health in the first place. Such programmes can help mitigate the massive mental illness burden that India faces. For instance, Raintree Foundation, which is funded by the Dandekar family, has adopted an integrated lens in its work. Its programmes focus on climate change and rural development while incorporating aspects of disability and mental health. Similarly, MHI supports and funds LAW Foundation, a Bihar-based nonprofit, in providing free legal aid alongside psychosocial support to incarcerated persons and their families. LAW Foundation believes that mental health care is not only integral to detainees’ rehabilitation and reintegration into society but also reduces the likelihood of relapse.
Currently, however, public funding for mental health care in India is predominantly allocated to tertiary care institutions, and primary healthcare centres are neglected. Despite CMH models offering cost-effective and efficient solutions that can reach remote areas, nonprofits struggle to attract funding and support for them. This is largely due to a lack of effective advocacy highlighting the effectiveness of CMH models. Moreover, India’s historical preference for institutionalised care further hampers funding directed towards community-based approaches.
3. Research and scientific programmes
In a third, distinct but linked manner, donors support research and scientific programmes by funding programmes at universities or healthcare institutes. For instance, in March 2023, Rohini Nilekani Philanthropies (RNP) made a grant of INR 100 crore to NIMHANS and the National Centre for Biological Sciences (NCBS) to set up the Centre for Brain and Mind.
The findings of such undertakings can influence and support interventions across the first two approaches in the future. The motivation here is to fund research and create credible data and knowledge rooted in the Indian context.

Several challenges hinder donors from giving more
Philanthropy in mental health presents significant complexity and is hindered by numerous challenges. Consequently, many donors prefer to partner with well-established institutions as a practical entry point in their efforts to support mental health. Especially for substantial donations, collaborating with institutes of excellence reassures funders that their contributions are being utilised effectively. However, our research revealed numerous additional barriers that impede both new and experienced donors from contributing to mental health causes in a significant way.
Stigma: Despite efforts from various stakeholders to raise awareness, mental health remains heavily stigmatised. It is often individuals who have lived experiences of mental illness who are motivated to give. However, this is a double-edged sword. On the one hand, donors give because they feel a sense of personal responsibility to act. On the other, it can deter donors who fear the stigma of association with mental illness.
Lack of a clear pathway: Indian philanthropists in sectors such as education or nutrition have access to a plethora of trusted experts, philanthropic intermediaries, case studies, evidence, knowledge, and understanding of desirable outcomes—all necessary for them to feel confident about giving. Unfortunately, mental health faces a dearth of relevant information and knowledge.
One reason for this could be the lack of intermediaries to bridge the gap between donors, experts, and nonprofits. This includes policy and research organisations that generate trusted and credible knowledge; collaborative platforms or convenings where best practices and learnings are shared; and advocacy entities that guide and influence government around macro-level change. The proliferation of these supporting organisations could spur giving in many ways, as it has, for instance, in education or climate change. Consider the India Climate Collaborative, which works on climate action. This collaborative has set up and seeded many platforms—such as Earth Exponential, Harit Bharat Fund, and Bharat Agroecology Fund—to drive and catalyse even greater funding and action toward solutions.
Capacity constraints: There are not enough nonprofits working on issues of mental health, which leads to an inadequate absorption capacity for funds. For donors, this poses difficulty in finding and funding the right partner to implement a programme in alignment with their vision.
India faces an acute shortage of trained psychiatrists, psychiatric nurses, psychologists, and other specialists, which further aggravates the issue. Additionally, addressing mental health issues effectively requires individuals who are sensitive to the sociocultural nuances of different communities and possess a diverse range of skills. These individuals could be teachers, doctors, journalists, police officers, lawyers, and community workers who have a deep understanding of the specific needs and cultural contexts of the communities they serve. However, organisations rolling out mental health programs often find it difficult to find the right talent for their programmes. Further, even after hiring, many organisations working in mental health often need to invest time and resources in training and upskilling their staff. This adds to both the cost and complexity of mental health programming.
Intangibility of impact: The impact of mental health interventions is not always visible or tangible, especially in comparison to other health issues, where donors can see the curative work that has taken place. Mental health outcomes are subjective and difficult to measure with precision; often, they are also integrated with structural determinants such as income levels, gender-based violence, and substance use. Additionally, mental illnesses do not always follow a linear path of detection, treatment, and cure; they can recur throughout a patient’s life, necessitating ongoing support and management.
Funders and nonprofits in India currently use a wide range of tools, both quantitative and qualitative, to understand the impact of their programmes. Globally, however, the narrative is shifting toward functional outcomes such as improved school performance, reduction in alcohol use, better physical health management, or sustaining employment in the long term. In the long term, the sector needs some convergence around the effectiveness of an intervention and general agreement around what constitutes success in mental health programmes.
Mental health is a complex and intersectional issue that will require change on various fronts and collaboration among many stakeholders. Most importantly, it will require funders to maintain a long-term perspective and accept that measuring outcomes and successes in this sector might differ significantly from other sectors that they fund. Philanthropy can play a pivotal role in fostering this long-term vision and bringing positive change and progress in the realm of mental health.
—