Most discussions about healthcare delivery start by celebrating the impressive gains made in tackling infections, and reductions in maternal and childhood mortality (even though we remain behind several countries with comparable economies). There is also a general agreement, reinforced by reports of the Global Burden of Disease Study, that future threats to population health and economy will come from the rapidly growing burden of chronic non-communicable disorders. We also agree that addressing the challenges presented by these conditions requires a qualitative change in the way healthcare is delivered.
Communicable diseases announce their presence by making an individual fall ill, which makes her want to seek medical care. In contrast, non-communicable disorders generally do not produce symptoms until major complications involving important organs – like heart attack, stroke, kidney failure or blindness – develop, which is generally too late. Non-communicable disorders like high blood pressure, diabetes and kidney disease may be discovered either during a routine health check or when she undergoes evaluation for an unrelated condition.
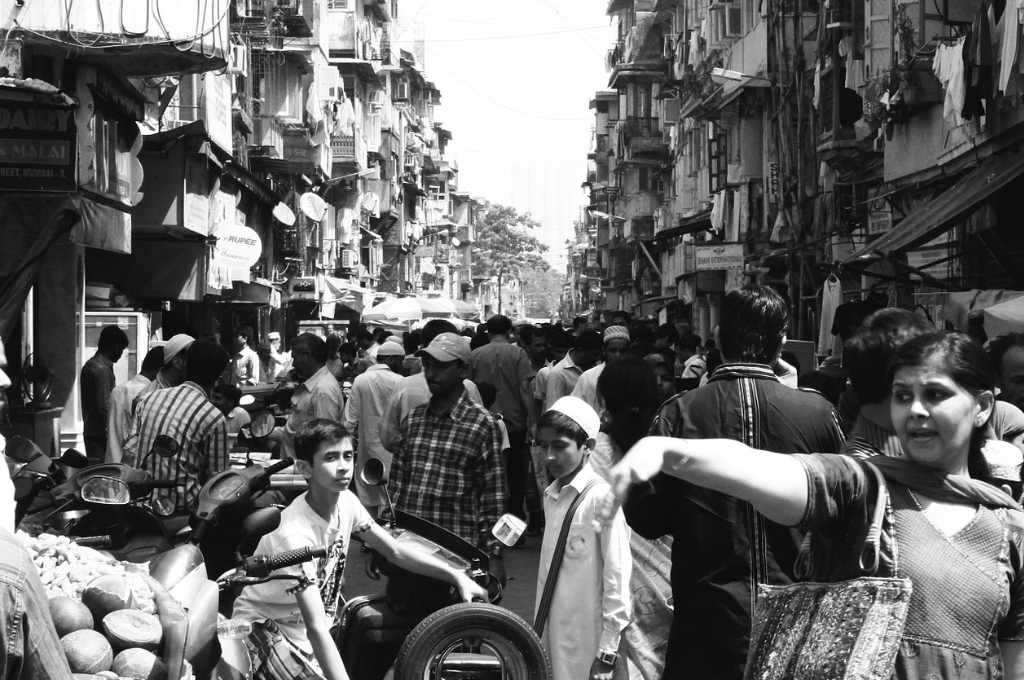
Competing priorities force her to the demands of daily life more seriously, and a disease that is not bothersome is ignored. Further, the main providers of healthcare are doctors, who are relatively scarce and always expensive. The need to repeatedly visit a faraway doctor for management of conditions that are likely to be present for a person’s lifetime is not a recipe for optimal sustainable care.
All stakeholders now agree that increasing penetration in care delivery for chronic noncommunicable diseases in emerging countries will require us to move away from the West’s physician-based models of healthcare delivery, which favours the relatively privileged. The democratisation of this process requires us to identify resources in the community and co-opt them to improve efficiency.
Related Article: Rural India is facing an epidemic of non-communicable diseases is rural India

Photo Courtesy: Charlotte Anderson
Importance of task-shifting
One such method is ‘task-shifting’, in which some of the basic services traditionally provided by physicians are delivered by community-based frontline health workers. These workers use well-defined care algorithms to identify and guideline-based tests to stratify individuals according to risk on the basis of simple questions and tests. This triaging allows health workers to provide essential basic advice based on best practice for disease management (short of drug prescriptions, since non-physician healthcare workers are not allowed to prescribe drugs in India), referring those who really need medical advice to doctors and regularly monitoring them for treatment adherence and control, at or close to their homes.
In addition to improving the efficiency of healthcare delivery in the community, technology-enabled task shifting frees up doctors’ time as well. Physicians can spend more time on critical thinking and decision making, and use targeted data, information and knowledge to make better decisions about patients and disease processes. They will provide oversight on quality, prevent over-reliance on devices, make sure the right amount of data is received (when it may not be), detect inaccuracies with monitoring devices and develop problem-solving techniques.
This approach is similar to the assembly lines of Japanese automobile manufacturers, and also McDonalds, where individuals use standard operating procedure to perform the same task over and over again – the result being a product of predictable and uniform quality.
Task shifting has helped bring the maternal mortality down in many developing countries, including India, and in managing HIV-infected individuals in Africa. Accredited Social Health Activists (ASHA), a group of young women from within the community, have been central to this phenomenon. With the advantage of having the trust of the community they belong to, they can enter people’s homes, bring down communication barriers and, importantly, reach groups that access healthcare less often – such as women.
Now, how can we provide health workers with the training and support to perform these tasks efficiently and without making mistakes?
This brings us to a much (ab)used term, called mHealth. The most widely accepted definition of mHealth alludes to the use of mobile devices for the delivery of healthcare. Though many innovations have been proposed and developed in mHealth, most fail soon after their evolution beyond the prototype stage because they have been designed as “solutions in search of a problem”. They focus on a single disease condition, place disproportionate emphasis on the technology and pay insufficient attention on health system integration and the socio-technical aspects of innovation.

Photo Courtesy: N i c o l a/Flickr, CC BY 2.0
Difficult but necessary
According to one estimate, over 400 health-related apps are being developed each month around the world. At last count, we found over 250 apps in the Play Store for Android phones just for diabetes management.
mHealth enthusiasts envisage healthcare delivery as an engineering problem, as if a technical solution can be developed to solve it. The enterprise also suffers from pilotitis: a large number of startups are coming up with-disease specific apps and launching them in the market without also generating robust evidence around their usability, efficiency, efficacy, cost-effectiveness and/or scalability.
A fundamental flaw of these solutions is an imperfect understanding of how these diseases kill and/or disable people. Individuals do not fall sick just because blood sugar or blood pressure are poorly controlled, but because these conditions increase the risk of damaging the functioning of some vital organ. This requires risk-based stratification to be implemented together with a management approach that consists of interventions working together to bring down the risk.
This in turn requires developers to understand how various risk factors intersect and so develop ‘bespoke’ solutions based on an individual’s risk profile. Modern information technology makes all this possible – its users only need to recognise the nuances of disease biology in addition to technology.
These electronic tools have additional benefits. They create a permanent electronic health record of an individual that allows a person to understand her health better and take a participatory role in tailoring care delivery. mHealth also allows us to monitor disease trends, track quality of care according to predetermined standards and help plan and allocate healthcare resources. As the volume increases, data about care and operations will translate into knowledge that drives evidence-based clinical practice and health system transformation.
To achieve scale, mHealth innovations need to be developed and evaluated in a real-world context and integrated within existing and emerging health systems, so that reliable evidence around effectiveness, cost-effectiveness, scalability and sustainability can be generated. Early steps in producing a scalable solution by applying a health systems perspective is crucial. Research has shown that although mHealth technology facilitates task-shifting and self-care, both of which can lead to affordable and scalable care models, this happens only when it is carefully developed within existing systems.
Publicly funded or commercial routes to scale these solutions up need to be explored. These steps are essential to demonstrate the efficacy, accuracy, acceptability and scalability of mHealth innovations. Unlike utility apps, health-related tools, products or innovations have a direct impact on the health and well-being of people.
mHealth-led approaches also hold promise for providing long-term care to patients with established chronic diseases through remote diagnostics and monitoring mechanisms, patient self-care technologies, managing therapeutic devices with the aim of improving quality of life, reducing hospitalisations and improving outcomes.
Some months ago, when Soumya Swaminathan, the then-director-general of the Indian Council of Medical Research was interviewed by The Wire on the eve of her departure for a new job at the World Health Organisation, she remarked, “If we can build Mangalyaan, why can’t we do more in health sciences?”
A statement like this makes for attractive copy. As a standalone technological task, it may be even simpler. However, understanding the almost limitless number of patient- and system-related variations and building the appropriate medical logic for the complex Indian healthcare system could test the hell out of the smartest rocket scientist.
Appropriately conceptualised solutions supported by technology can have lasting impact on long-term community-based management of chronic conditions, reduce inefficiencies caused by disease-specific silos of healthcare delivery and narrow health outcome disparities. Short-cut approaches are all a road to perdition.
This article was originally published on The Wire.