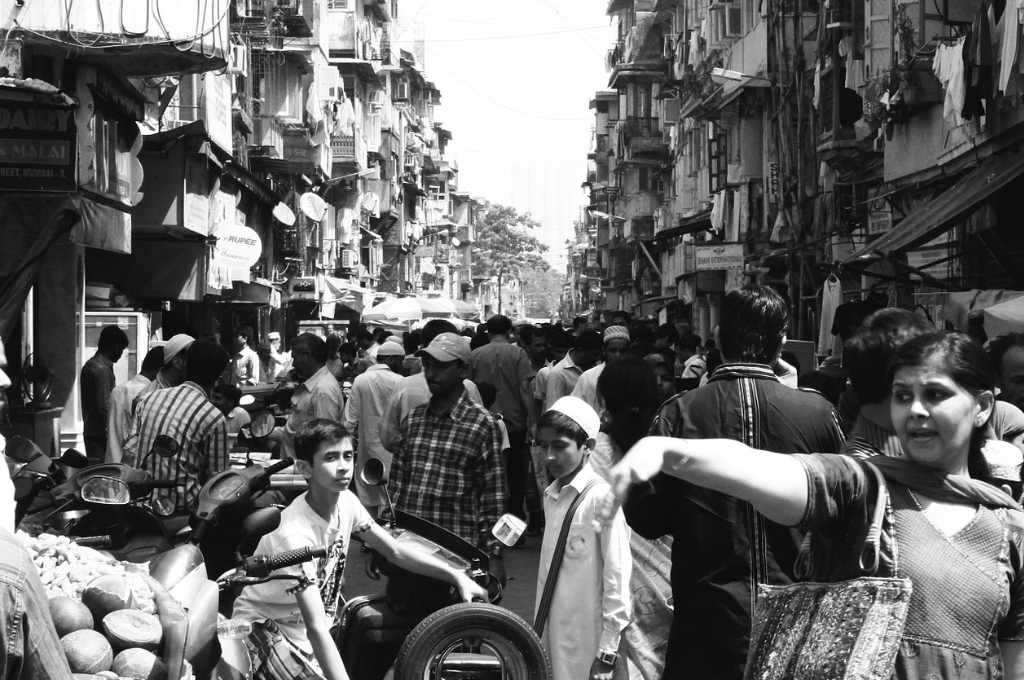
Historically, the delivery of high-quality primary healthcare in India has been hindered by a number of challenges: low budgetary allocations, limited access to primary care facilities, shortage of doctors, and regulatory challenges, among many others.
But over the last five years, India has seen significant tailwinds driving improvements in access to primary care in the country. In 2017–18, the government put forth a new National Health Policy, which highlighted the importance of primary healthcare. It also mandated the creation of approximately 1,50,000 health and wellness centres with the objective of bringing primary care within walking distance for every individual. In particular, these were meant for rural and remote areas with little access to primary care due to which patients often had to travel large distances for basic facilities. More than 1,30,000 health and wellness centres have already been operationalised across the country and the figure is expected to hit 1,50,000 by the end of 2022. In parallel, the government is creating a digital health infrastructure through the National Digital Health Mission (NDHM). The NDHM aims to build the digital infrastructure to support data management, create health IDs, and create seamless payment architecture with insurance companies and private providers. The government has also announced the opening of more than 100 new medical colleges by upgrading the district hospitals.
So, with efforts being made to narrow the access gap at the policy and operational level, what must the government focus on next to build a high-quality public health system?
1. Build sustainable partnerships with private sector to drive innovation
In the last eight years, the government has focused on improving access to healthcare facilities for the marginalised through programmes such as Ayushman Bharat PMJAY (which provides health insurance cover to low-income households) and Ayushman Bharat health and wellness centres (which provide primary care in rural and remote areas). Simultaneously, the private sector has been driving significant innovations in improving diagnostics, therapeutics, and quality of care using technology such as AI and machine learning. With these two very complementary strengths, it remains to be seen how these two actors can work together.
During the pandemic, we saw many successful examples of collaboratives unifying the public and private sectors and working successfully at scale. The Swasth Alliance, Feeding India, and ACT Grants collaborative brought together many donors and implementation partners during the catastrophic second wave of COVID-19 to procure and donate approximately 50,000 oxygen concentrators across India. Using a committee structure, the collaborative worked closely with Government of India stakeholders—such as MyGov.in—to ensure that public facilities most in need were served first. Academic institutes such as IIT also provided technological and analytical support. The development of the CoWIN portal is another example of how the private sector supported the government’s COVID-19 vaccination drive.

2. Shift the focus from activities to outcomes—we fix what we measure
While the current focus is on bridging the access gap and setting up a strong health infrastructure, it is equally important to think through a robust framework to track the progress and longer-term outcomes from these new initiatives. A well-designed primary care system can reduce the burden on secondary and tertiary care systems, improve national productivity, and reduce overall cost of care in the country. It is critical to set up systems early on to track progress and enable decision-making, based not only on outputs and activities but also on outcomes. This ensures that course correction can happen early on and is based on real-time data, and that high-quality interventions are prioritised.
India is already witnessing progress on this front: for instance, the Development, Monitoring and Evaluation Office of the NITI Aayog has recently come up with an output–outcome framework, which tracks budget spending against output and outcome metrics across multiple ministries, including the Ministry of Health. The logical next step would be to amend policies to change budgetary practices. This will allow government bodies to budget and pay for outcomes—as opposed to inputs and activities—wherever possible. To see how these frameworks support decision-making in practice, we need strong pilot programmes in the primary healthcare space.
Another example of how outcomes-based tools can be used to improve decision-making is using financing tools, such as impact bonds. Under an impact bond, an investor provides upfront funding to set up and run a programme towards achieving pre-agreed outcomes with donors (also called outcome funders). If the agreed outcomes are met and verified by an independent evaluator, the investor is paid back the capital with a pre-agreed rate of return by the outcome funders. As a result, this tool creates a financial incentive for the investor (and therefore the service provider who they fund) to drive focus on delivering outcomes, and creates a controlled environment under which they can use innovative tools or approaches to drive outcomes. India is also seeing strong early examples in this space—the country’s first health impact bond, the Utkrisht Health Impact Bond, aimed at improving the quality of 500+ healthcare facilities to achieve national accreditation standards and the quality of maternal care and childcare provided. In 2021, the bond completed operations and saw successful results overall. It improved the quality of care in 405 private healthcare facilities throughout the state of Rajasthan, reaching more than 4,50,000 mothers and newborns, and saving more than 13,000 lives in a five-year period.
3. Prepare now for future crises
Climate change is now perhaps the single biggest health threat facing humanity. Increasingly frequent extreme weather events, pollution, and zoonoses are impacting health and well-being in multiple ways, often resulting in illness or death. Emerging evidence from a review of 36 epidemiological studies from around the world suggests that more extreme temperatures—especially high temperatures—are also associated with preterm birth, low birthweight, and stillbirth. Air pollution has also been shown to increase the risk of low-birthweight infants and preterm birth. Apart from impact on maternal and neonatal health, climate change is expected to affect broader health and mortality rates as well. According to a study, by the end of the century, climate change may increase the mortality rate due to excessive heat by six times. There is now ample research on how climate change and healthcare are inextricably linked. The recent COP27 discussions also underscored this: The COP27 Health Pavilion emphasised the importance of placing health and equity at the centre of climate negotiations.
As adverse weather events become more common, the dependence on a strong first point of care is only bound to increase. It is now critical to prepare our primary healthcare systems to both deal with climate-related emergencies as well as work closely with communities on mitigating and dealing with climate change–related challenges. For example, having a more targeted set-up of primary care clinics in areas prone to flooding or forest fires, training their staff to deal with weather-related emergencies, and supporting them with emergency supplies and technology to manage crises when they arise. Improving quality of care to deal with the constantly evolving challenges of climate change is no longer a want, but a critical need for the future.
An agile and strong primary healthcare system is critical to meeting the SDG goals and ambitious COP27 commitments. The progress that India has made in terms of improvement in access to care in the last few years has been quite noteworthy. Both the public and the private sector have also learnt many lessons during the pandemic. It’s now time to leverage these gains in response to the challenges that lie ahead.
—
Know more
- Listen to this podcast to learn about how the public and private sectors can fix the gaps in India’s healthcare system.
- Understand how India’s health crisis is pushing people into poverty.
- Read about why the government needs to include private healthcare providers into its digitisation efforts.
Do more
- Connect with Krisha Mathur at krishamathur@gmail.com to learn more about and support her work.