This is the story of an itch.
It is set in the tribal villages of Gadchiroli—a remote, semi-tribal district located in central India.
The year was 2006. Like in every other year, the climate was hot and humid with heavy rainfall, and tribal people from several villages were repeatedly complaining of ‘itching’. Though it is a common health complaint, the magnitude of itching, they told us, was unprecedented in 2006.
Usually in this community, itching was caused by scabies; therefore, trained Community Health Workers (CHW) of SEARCH (Society for Education, Action & Research in Community Health), the organisation I was working with, were treating people with standard scabies medications, but to no avail. The cause of this mysterious spurt in itching remained unknown.
What follows is an account of our investigation into this condition and what it taught me, a young medical graduate who had then just started working in these tribal villages, about how to approach a community—its culture, ecology, and the problem itself.
We were curious about why this sudden outbreak of itching, which one intuitively associates with poor hygiene, had occurred, because tribal communities are known to be scrupulously clean, personally and as a community. Hence our team, consisting of myself, several non-medical health supervisors and tribal village volunteers, decided to study a village—Gathanyeli—in-depth to try to ‘re-search’ a community we had known so well, to identify the cause and how we might help it abate.

Photo courtesy: SEARCH
A curious case of itching
Gathanyeli is five kilometers from the main road, 15 from the nearest primary health center, and 50 kilometers from the District Hospital. Only a kaccha road provided some connectivity, a road which would invariably be under water during the monsoon. It had twelve houses with a total of 60 inhabitants. The main livelihood was paddy cultivation during the rainy season and selling minor forest produce such as Bamboo, Tendu leaves (Diospyros melanoxylon, the key ingredient in bidis), and Mahua (Madhuca longifolia)—flowers collected from the surrounding dense forest.
[quote]We were faced with a wide-ranging diagnoses profile, and decided to conduct an environmental study of 12 households to delve deeper.[/quote]We examined all inhabitants present in the village, several of whom were children. Clinically, several morbidities such as Scabies (the most common), skin infection, fungal infection, head lice and dandruff, insect bites (especially mosquitoes), and allergies were present, all causing itching. In fact, most individuals had multiple conditions. So, we were faced with a wide-ranging diagnoses profile. Hence, we decided to conduct an environmental study of all 12 households in order to delve deeper.
Related article: Rural India faces epidemic of non-communicable diseases
What we learned
As expected, everyone was bathing daily, some in fact twice. Almost all were using soap. But because many didn’t have private bathrooms, their private parts weren’t well washed, especially in the case of women. Men were bathing in the nearby stream, along with cattle, which exposed them to insects. To scrub their bodies, they were using small sharp stones, which caused abrasions, increasing their likelihood of skin infections.
In most houses, the family was using the same hairbrush, transmitting hair lice easily. The linen was commonly exchanged, so scabies would spread rapidly too.
In tribal communities, menstruating women live in huts called ‘Kurma’, which lack proper shelter, making it difficult for the women to bathe properly. They sleep on a mud floor. Living together for four to five days in a small, unclean, humid hut further spreads scabies and fungal infections.
Tribal houses were mini zoos, with dogs, cows, buffaloes, hens, cocks, goats, pigs, ducks, parrots, pigeons, and sometimes deer living inside. In some houses, we even found bats. Dogs, hens, and ducks slept on the same bed as the family members. This allowed for easy transmission of lice and ticks.
Paddy was also stored in the bedrooms, and the husk possibly causing allergic itching.
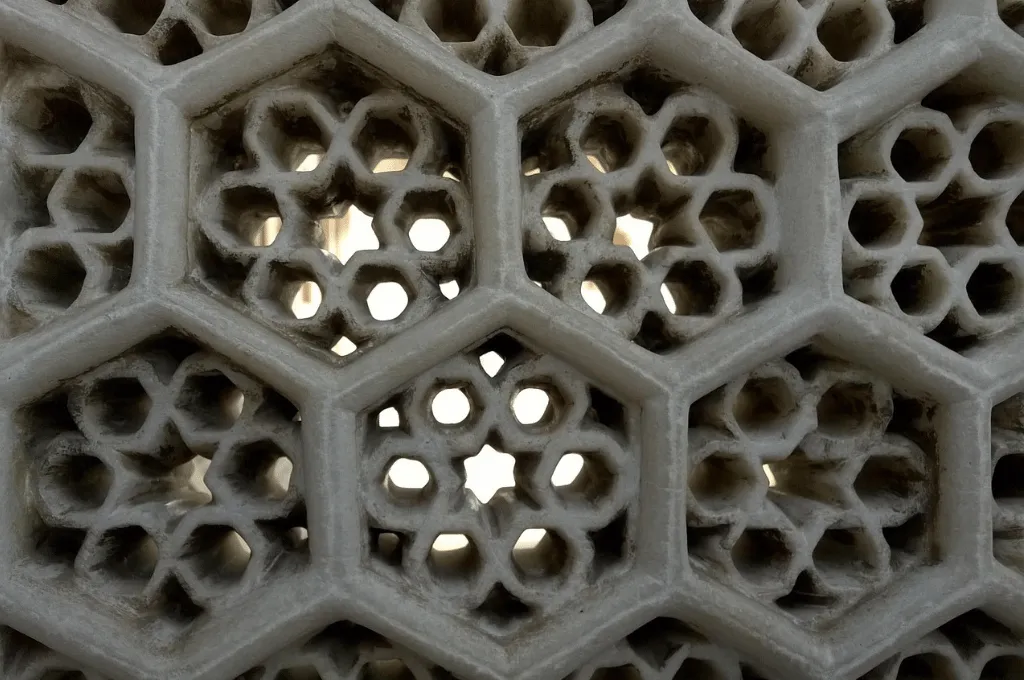
The mud flooring and walls allowed water to soak in, and so, especially during the monsoon season, houses remained wet and humid. Most of the rooms had no windows. This was not uncommon in tribal communities because windows provide open access to predators or snakes and were also impractical during the rainy season. The drawback of this though was that it was cutting off any ventilation or natural light.
In all the houses clothes were washed daily using detergent, but in most houses clothes were dried under the shade, shielded from the sunlight. Hence, even clean clothes remained sticky and wet. When asked why they were avoiding the sun, they explained to us that heavy winds would cause their clothes to fly away if left out in the open.
Further confounding the issue was the immediate environment of these tribal households. The courtyards had small, open water tanks full of algae and dirt, and were the ideal breeding ground for mosquitoes. Needless to say, people complained of constant mosquito bites, leading to vigorous scratching with dirty nails, causing infections. And why were the tanks not emptied daily? Because there was no water source nearby, creating a state of continuous water insecurity.
People also reported that three varieties of vegetables and grass—commonly found in the field and surrounding forest—were causing itching, as was working in the rice fields. But obviously, there was no escaping farming or the forest, given that it was their main source of livelihood.
Not only were there a large variety of causes for the itching, but once diagnosed, compliance with our medication regimen was also an issue. For instance, our CHWs had offered scabies medication—Gamma Benzene Hexachloride (GBHC), but its use was inappropriate. Some were not applying the lotion to their private parts while others stopped using it entirely because it caused a stinging sensation.
The CHWs also advised people to bathe with hot water after applying GBHC, but because hot water exacerbated the itching, people stopped using it. It became a vicious cycle as GBHC is a cure for scabies, but because of partial compliance with the CHWs recommendations, results were limited. This decreased people’s confidence in the CHWs and further impacted their inclination to comply, and increased their complaints.

Photo courtesy: SEARCH
We were still left with the question: What made this year different?
Instead of only focusing on an individual, we tried to fathom the reasons within the overlying ecology.
First, the rainy season was longer than usual, with the rains being distributed over many months rather than concentrated in a shorter time window. This left no dry days and a constantly overcast atmosphere, which meant that wet clothes did not dry and ponds in cattle sheds remained stagnant with continued mosquito breeding.
Second, the veterinarian doctor serving these tribal villages had disappeared for reasons unknown, leaving most cattle untreated. So, zoonotic transmission of infections from animals to humans remained unchecked.
Third, most of the vegetables that were causing allergic itching had been distributed by the government as subsidised crop some time back, which was now harvested and caused allergic reactions.
Fourth, children were running away from their tribal residential schools and returning home more often that year, probably due to worse than usual administration in these schools. Because they had contracted scabies and lice in their schools, those conditions were now spreading in their villages. In fact, in many homes people themselves traced the start of itching to an index case—the returning child.
Finally, though Gadchiroli had been ravaged by the violent, ultra-leftist insurgency for many years, that year in particular, the Naxalites were organising repeated strikes against even farming. This meant that the communities had to shift their cultivation schedule. As a result, they were more exposed to rain and insects in the farms.
Related article: IDR Interviews | Dr Rani Bang
This was a unique situation
Instead of only focusing on an individual as a clinical case, we found ourselves trying to fathom the reasons for a condition within the overlying ecology. We had to decipher the interaction between factors including environmental (climate, plants, farms, and houses), human (personal, occupational, societal, habits and traditions), and vector (mosquito and cattle), all of which ultimately converged and contributed to the health challenge.
Hence the seemingly paradoxical observation: bathing daily and scrubbing the body, washing clothes regularly, sending children to school, and the distribution of plants by the government were all contributing to itching.
As treatment, we conducted clinics in many villages and demonstrating the ideal method of using GBHC, ensuring its mass application. We also administered antibiotics, anti-fungal, and anti-allergic medication, in addition to GBHC, to treat the several other causes of itching, and not just scabies. Focused health education was provided pertaining to several of the behaviours. The hygiene of the cattle shed was improved and water tanks nearby were emptied, eliminating the mosquito breeding sites.
Soon reports started reaching us that the problem had abated. The following year, the rains were regular, the ultra-leftist movement had stopped calling strikes against cultivation, scabies was aggressively identified and treated, and people in general were more aware of the different causes of itching, seeking treatment. There was no recurrence of the itching epidemic.
For me, this was a journey of discovery
Though I had joined our team at SEARCH recently, we as an organisation had been working with this community for more than a decade. We thought we knew them—their health, their challenges and their environment—so well. And yet, through this micro-study in a village, many new lessons emerged.
Much like the Gandhian approach to change, we must focus on evolution and incremental steps rather than a complete revolution.
For me, it was also a great first hand insight into the difference between clinical medicine (inside the hospital) and public health (inside the community) as to just how many related and seemingly unrelated factors were contributing to causing something as innocuous as itching. Prima facie, the ideal solution seemed to involve a complete change of tribal lifestyle, ranging from building houses with proper ventilation and sunlight, and cement flooring in neighbouring cattle sheds, to administering an easier-to-use medicine than GBHC, improving governance, and bringing peace in an insurgency-affected community.
Of course, solving the problem doesn’t mean we must try every single solution mentioned above. I have learned that instead, we must identify solutions based on our abilities, and much like the Gandhian approach to change, focus on evolution and incremental steps rather than a complete revolution.
Looking back, I recollect the vivid memories of those tribal children, initially fearful, full of lesions and pain, but joyously coming to meet us just a few days later. In serving them, I received the answer to the question: Whose Am I?