I am an occupational therapist at the Jai Vakeel Foundation, a nonprofit that works with children and adults with intellectual and developmental disabilities (IDD).
Children with disabilities are amongst the most marginalised and excluded groups of children and experience widespread violations of their rights. At Jai Vakeel this means working with children whose IQ is under 70 (the normal range of IQ is 90-110). In addition to deficits in adaptive behaviours that affect their everyday life, most may have other associated disorders such as autism, epilepsy, cerebral palsy, or visual and/or hearing impairments. Occupational therapy is a paramedical field in which we teach an individual how to adapt and access an education and an occupation, in the places where they live and work.
Before the COVID-19 crisis struck, I would spend five days a week at our school campus in Mumbai, conducting therapy sessions. The objective is to help our children achieve some level of functional independence or self-sufficiency—this could mean the ability to walk, eat, or dress independently. Self-care skills play a major role in a child’s overall functional growth, confidence, and independence.
It is not unusual for children with IDD to be segregated—in their communities and sometimes within their families as well. Our goal is to ensure a child’s social inclusion, and helping them to be self-sufficient is a critical step to enabling their inclusion in their families, communities, and society at large. Engaging and empowering parents is central to our intervention.
COVID-19 has exacerbated the equity issues that our students and their families face, as more than 40 percent of our students come from the lower income strata. In the early days of the pandemic, the well-being and safety of our children and families was our priority. We provided 354 grocery kits with daily essentials and 59 medicine kits which are critical for our students.
As the reality of the pandemic settled into our daily lives, we adapted to create a new kind of stability: We re-imagined our department goals; Zoom, Skype, and WhatsApp calls became our therapy rooms; and we made parents our partners to ensure that our children’s therapy needs were met.

Before the COVID-19 crisis struck, I would spend five days a week at our school campus in Mumbai, conducting therapy sessions. | Picture courtesy: Jai Vakeel Foundation
9 AM: I start my day by reviewing the schedule of the day’s sessions, which we prepare and share with each child’s parents the previous night. I usually take six to seven sessions in a day, with each lasting for 45 minutes. I tend to schedule sessions with children who may find it difficult to cooperate, towards the end of the day. This way, if I need to spend more time with them, it doesn’t affect other sessions.
9.30 AM: My first session of the day is with Abhay*. From his earliest days his milestones were delayed, leading to issues with head holding, eating, crawling, and walking. He was unable to communicate and was completely dependent for feeding and all his other needs. A firm diagnosis and appropriate treatment evaded the family for many years.
At age eight Abhay was finally diagnosed as autistic by our medical doctor, along with moderate intellectual developmental disability. Our team has worked closely with Abhay and his mother since 2017, and today he can communicate with his family and close caregivers with expressions. He can convey his moods, his needs, and his happiness. He can also walk across a room—his mother’s greatest joy.
In addition to coping with the shift to virtual therapy, many parents were concerned about how they would replicate therapeutic materials at home.
His mother is now keen that he learns how to eat independently with a spoon. In order to achieve this goal, we start by practicing some basic activities such as moving the spoon around in a bowl of water, using the spoon to transfer pulses from one bowl to another, and so on. It will take us several months of practicing these actions before he advances to feeding himself with a spoon, independently.
Today’s session goes well, and Abhay’s mother and I are both happy with his progress.
While Abhay was very cooperative during therapy sessions at school, he found the shift to attending remote sessions quite challenging. He became non-compliant, easily distracted, and hyper. It was extremely challenging to have him focus on the task at hand. His mother and I have spent many sessions working on this—providing him with bite-size activities and giving him lots of breaks in between. Over time, our efforts have paid off and Abhay has learnt to stay focused.
When we first started conducting sessions remotely, we faced many such challenges. In addition to coping with the shift to virtual therapy, many parents were concerned about how they would replicate therapeutic materials at home. And so, along with parents, we came up with ideas of how to use objects and materials that are easily available at home, in therapy. For instance, we have replaced bead-stringing with stringing pasta or pieces of play dough. After we gave parents a few ideas, they started suggesting many others of their own. One mother has been giving her child a lock and key to play with, to improve hand movement and fine motor skills. Other parents are setting up activities such as throwing a ball into a bucket to improve gross motor skills.
11 AM: Over the course of the next session, it becomes apparent that we will not be able to complete this session as the child, Savitri*, has a meltdown and refuses to comply. Savitri is seven years old and has Severe IDD with Autism Spectrum Disorder (ASD) and Attention Deficit Hyperactive Disorder (ADHD). She exhibits constant hand flapping, jumping—sometimes for hours, running around continuously, and severe vocal stimming (continuously making noises). She has received a range of different interventions including behaviour therapy and counselling, and has been on medication for her restlessness and ASD symptoms.
She had her first seizure during lockdown, causing her mother to experience high levels of distress and anxiety. In consultation with our medical director, she had an EEG taken. Since then, Savitri has been on medication to control her seizures and has now stabilised. Her mother has also been receiving regular counselling sessions to help calm her own distress.
Since we cannot complete the session together, I let Savitri’s mother know that I will share some videos with her from our digital content library on YouTube that will help her provide Savitri with a ‘sensory diet’ throughout the day. I also ask her to record a video of Savitri doing these activities and share it with me, so that I am aware of her progress. I make a note to speak to our counselor to schedule another session with Savitri’s mother soon.
Despite the many challenges that we face during remote sessions, they have given us a peek into what actually happens when a parent tries to engage in therapeutic activities in a home environment. We now understand the realities of their homes better—11 family members living in cramped quarters, distractions such as others watching TV, talking on the phone, or arguing. We are also able to see exactly how others in the family interact with the child—earlier we would merely hear about this. This enhanced understanding of our children’s home environments has helped us tremendously in formulating therapy methods based on their individual needs.

I have worked as an occupational therapist for 22 years and never dreamed of having to impart therapy from a distance, but these last few months have really highlighted to me that where there is a will, there is a way. | Picture courtesy: Jai Vakeel Foundation
12.00 PM: It’s time to log on to our weekly department meeting via Zoom. I am part of Jai Vakeel’s healthcare department—a multi-disciplinary team comprising of psychologists, physical, occupational and speech therapists, and a neuro-paediatrician. We meet virtually, on a weekly basis, to share our experiences, discuss our challenges, and collectively find solutions for them. Most children who are in therapy need support from multiple therapists, and therefore we come up with ideas on how we can leverage our collective to best meet the needs of our children.
1.00 PM: I take a break for lunch, attend to some household chores, and check in with my daughter who is also studying remotely. She is in the tenth standard and it’s important that I make the time to support her through this critical year. My husband and daughter’s support over the last few months has allowed me to manage the extended and unpredictable working hours.
Therapy sessions continue through the rest of the afternoon.
3.45 PM: I am excited about my next session. It’s with Ria*, a ten-year-old diagnosed with epileptic encephalopathy resulting in epilepsy, severe IDD, and cerebral palsy of all four limbs. When she joined us two years ago, Ria was unable to sit or maintain head or muscle control. She has had two long breaks in her therapy owing to her mother’s poor health.
Ria defies her medical condition with her enthusiasm and spirit. It took us more than a year of active therapy to improve her head-holding ability and be able to sit in class. This seemingly small improvement has been life changing not just for her, but her mother as well, who now instead of constantly having to hold her head up is free to engage in other activities.
At the end of the day there is preparation for tomorrow as well as assessing each student’s care.
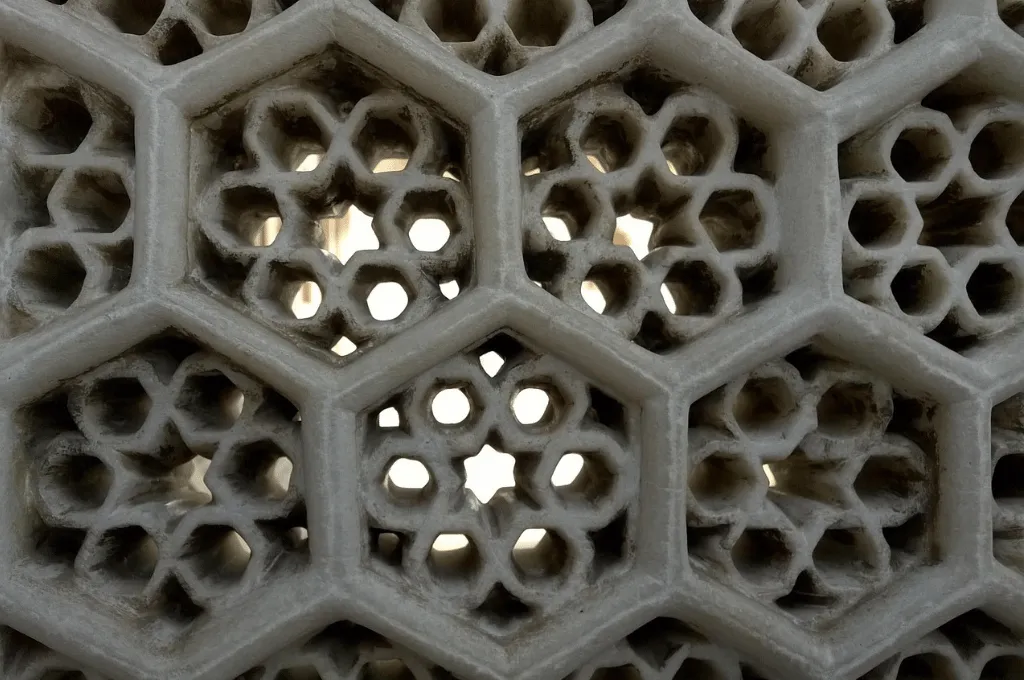
Before the lockdown, we had measured Ria and six other students for an orthosis—an external support that is prefabricated to the child’s specific needs and improves their ability to move independently. Since we cannot give parents hands-on training, we made videos that demonstrate how to wear and remove each orthosis correctly.
In today’s session, I work with Ria on muscle strengthening exercises—squatting, standing up from the sitting position with support, remaining in the standing position for five seconds while holding a football in her hands, and more. The session goes very well—the orthosis has given Ria the confidence and strength to stand up independently for five counts. Her face lights up. To see her smile is like sunshine on a rainy day! It fills the room.
6.00 PM: At the end of the day there is preparation for tomorrow as well as assessing each student’s care.
I have worked as an occupational therapist for 22 years and never dreamed of having to impart therapy from a distance, but these last few months have really highlighted to me that where there is a will, there is a way.
*Names changed to maintain confidentiality.
As told to IDR.
—
Know more
- Learn about intellectual and developmental disabilities.