The district of Gadchiroli has 1.2 million people, spread across 1,500 villages and three towns. A district sample survey we carried out in the years 2015 and 2016 showed that 41 percent of men had consumed alcohol in the past 12 months, spending a total of INR 80 crore. In the case of tobacco, 44 percent of people from across the district—men, women, and children—had spent annually a total of INR 298 crore of their own money on their addiction.
The annual district plan of the government in the same year was INR 157 crore, less than half of what poor people were spending, out of their own pockets, on tobacco and alcohol. This brought to light an interesting yet sad insight: tobacco and alcohol not only harm health, but they cause poverty.
Alcohol addiction
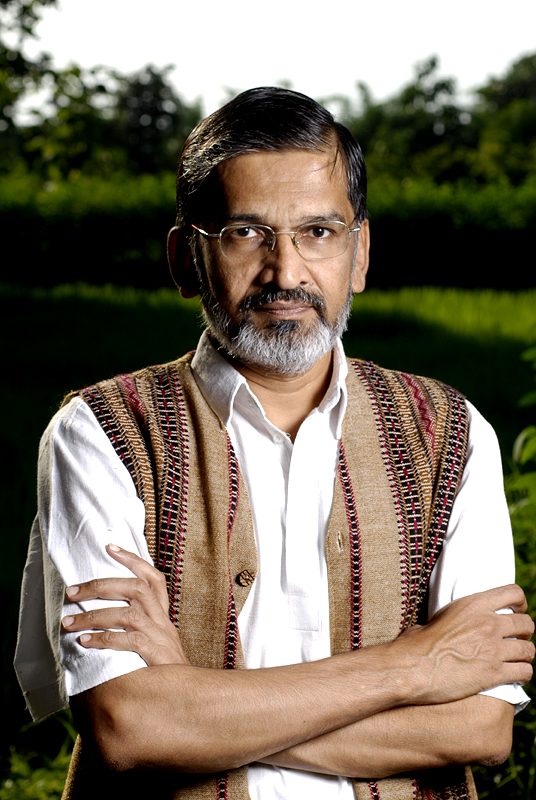
My first encounter with addiction was in the form of an alcohol addict, who was my driver’s brother. An ex-teacher, he had developed cirrhosis of the liver; his entire abdomen was full of water. I treated him but knew the prognosis. Within six months, he died. My second patient was a tribal man, who used to be an MLA. He too had cirrhosis of the liver. Within two months, he passed away.
I realised then that medical treatment was a futile solution for alcohol addiction.
These were frustrating experiences because I had never dealt with alcoholism as a clinical problem so directly. I realised then that medical treatment was a futile solution for alcohol addiction.
It was around this time that (Dr) Rani and I, would travel to tribal villages across the district, treating people and spreading health education. Everywhere we went, women would tell us, “Dr Sahib, aapki davai baju mein rakhiye. Hamari bimaari ke baare mein baat kariye (Doctor, set your medicines aside. We want to talk about our illness).
“Aapki bimaari kya hai?” (What is your illness?)
“Our husbands drink,” these women said. “Can you do something about it?”
We didn’t have an answer.
In Porla village, where Rani and I had organised a health camp, women started describing how their fathers used to beat their mothers under the influence. “My father would drink. My husband drinks. And now even my son has started drinking.” We knew that something ought to be done.
Women’s first problem is alcoholism of the men in their lives.
Across all villages we visited, women were very insistent. In fact, wherever I have travelled in India since, I have not yet found a place where women’s first problem isn’t alcoholism of the men in their lives.
As doctors, Rani and I wondered what we could do; alcohol after all was a political and social issue.
The scientific origins of alcohol addiction
There are primarily three causes behind succumbing to addiction. There can be a genetic tendency. Familial influence by way of normalisation of drinking can also play a role. And, in societies where a larger number of people take their first drink, we see a larger number of alcoholics. In fact, one of the most important factors that determines the magnitude of the problem in any society is how many people take the first sip. In the case of tribals succumbing to addiction more easily than non-tribals, the influence is largely cultural. We see this across different regions of the country, as well as among tribal populations in other parts of the world.
This is why we always listen to the people first. Scientific evidence keeps changing, but people’s life experiences—often, though not always—reveal the truth. According to the 2017 GBD, alcohol and tobacco are two of the top 10 causes of death, disease, and disability. Fifty years ago these substances were considered harmless, and were consumed for pleasure, but in terms of their health consequences, they are the cholera and plague of our times.

In 2015-16 across the district, men, women, and children, had spent annually a total of INR 298 crore of their own money on tobacco | Photo courtesy: Wikimedia Commons
The beginning of a 30 year struggle against alcohol and tobacco
In 1988, youth from the villages of Amirza and Wasa, came to us wanting to stop alcohol consumption in their villages. I told them to get the villages together and collectively impose a ban on it. At the time, I didn’t think they would succeed. But one month later, they returned, successful. They had organised people, and because women too were on their side, they managed to impose fines for both consuming and brewing alcohol. The youth would patrol village routes in the evenings to catch culprits.
We used these two examples to get other villages on board. Slowly, this snowballed into a movement.
Alcohol and tobacco are two of the top 10 causes of death, disease, and disability.
On October 2nd, 1992, we held a daru mukti sammelan, which was attended by 10,000 people from across the district to demand prohibition from the Government of Maharashtra. A people’s movement for daru mukti—liberation from alcohol—had been growing in the district for the past six years, and had spread to 150 villages. We warned the government that if it didn’t act, we would introduce People’s Prohibition. Finally, the government accepted our demands.
From 1993, official prohibition was introduced. Shops were shut and permits cancelled. Even though consumption reduced, rigorous implementation of the ban did not take place. Alcohol started entering through the borders of neighbouring districts. And because mahua—a local plant used to brew alcohol—was available in large quantities, people began brewing at home. After one year, a crude assessment told us that the net consumption of alcohol in the district had reduced by 60 percent. Forty percent had remained.
Was this a success or failure?
Thus far, our efforts at stopping alcoholism treated men as criminals. Fines were imposed upon them. In some villages, women shamed them by making them wear bangles in public. A close friend and social activist, Anil Awachat, prompted us to shift our perception of them from criminals, to victims. Realising that addicts were, in fact, chemical slaves, we decided to treat them rather than punish them.
We were prompted to shift our perception of them (men addicted to alcohol) from criminals to victims.
In 1994, we started conducting a 12-day residential camp for treating and counselling patients, with follow-up for one year. This seemed to work. After one year, the sobriety rate was 50 percent—a positive outcome for this disease.
Over the next 10 years we treated 4,000 addicts; of these, half slipped back into alcoholism within one year. At the three year mark, only 30 percent were sober. Hence while this programme was useful, it was no panacea.
By now, it had been close to 15 years that we had been fighting addiction, and all we had were partial solutions. Worse still, tobacco—a more insidious addiction—was on the rise.

“We warned the government that if it didn’t act, we would introduce People’s Prohibition” | Photo courtesy: SEARCH
A new villain
One evening in 2006, Rani and I were passing through the tribal village of Yerkad. There was a hand-pump by the side of the road, where an eight year old tribal girl was cleaning her teeth. I was very happy; after years of working in this area, I thought, school children had become so enlightened that they were cleaning their teeth in the evening. I got out of the car to praise the girl.
There were some tribal women watching me and laughing; they said that the girl was crazy. She cleaned her teeth every two hours!
I saw that she was cleaning her teeth with nus, or tobacco powder. Because she had become a nicotine addict, she needed tobacco every two hours. Here I was, thinking she was cleaning her teeth for oral hygiene; the women around us thought she was crazy, when in reality she was just a victim of addiction.
Around this time, we learned from our field staff about a new social phenomenon; increasingly, women were seen queuing up daily at 6 am at the paanthela (local paan shop), waiting for it to open. Earlier, this never happened. Having exhausted their stash at night, women would show up first thing in the morning for a fresh dose. The most prevalent form of tobacco consumption was oral—gutkha, kharra, nus, and gudakhu.
We estimated that people were consuming tobacco worth INR 73 crore per year, more than the total district government spending on NRHM, ICDS, and MGNREGA together.
A survey we ran in 2007-2008 in four blocks showed that 51 percent of people were consuming tobacco. When we extrapolated the money they spent on buying tobacco products, to the entire district, we estimated that people were consuming tobacco worth INR 73 crore per year. The prevalence was highest (60 percent) among tribal adults, and least (26 percent) in urban areas. In the very same year, the district had spent INR 10 crore on rural health, (NRHM), 14 crore on ICDS, and 22 crore on the MGNREGA scheme—the three national schemes for the welfare of the poor. But people’s spending on tobacco was more than the total government spending on these three schemes together.
We started working against tobacco. We worked with self-help groups, using the messaging: ‘Quit tobacco, save money’. We conducted a controlled field trial in three blocks which included health education, home visits, and so on. After one year, we saw a 15 percent reduction among women; (among men, it was three percent). We then tried working with children, thinking they would be an easier target. We ran a controlled trial in 50 schools working with children and teachers. After one year we saw very little effect.
Mere awareness generation didn’t work much against addiction.
The clinical approach had failed. Prohibition was only partly effective. The same was the case with alcohol de-addiction. And with tobacco de-addiction in particular, our efforts had been even less effective.
Where were we going wrong?
Two years of reflection on these frustrating results brought me to the realisation that thus far, we had worked on either supply or on demand, in isolation. We needed an integrated approach.We needed to fight both tobacco and alcohol simultaneously, while focusing on both demand and supply reduction.
To reduce supply, we needed to implement the government ban more rigorously, and mobilise communities to impose the village ban. To address demand, we needed to increase awareness so people wouldn’t start consuming either substance. And for addicts, we needed to work on de-addiction. Thus emerged a four-pronged, integrated strategy.
To implement it, we needed to work with the government, rather than against it, we needed to also work with non-government actors, and of course, the community, which is the most important stakeholder.
This was no longer an issue of addiction alone, but of development. Addiction is not just a health issue, but also a women’s issue. Both alcohol and tobacco produce poverty.
I took this four-pronged approach to the Chief Minister of Maharashtra. By then we had done two district sample surveys (2015 and 16) in which we found that the people had spent in one year a total of INR 378 crore on purchasing tobacco and alcohol. This was no longer an issue of addiction alone, but of development. Addiction is not just a health issue, but also a women’s issue. Both alcohol and tobacco produce poverty.
This programme—Muktipath—we launched with the partnership of the state government and the partial support of the Tata Trusts. The district pilot is currently underway in Gadchiroli. In three years, Muktipath aims to reduce prevalence of both substances by 50 percent, and reduce out-of-pocket expenditure on both by INR 100 crore per year.
Thus far, we have seen a momentum build across the district, from widespread awareness and community bans on drinking or selling alcohol across 600 villages, to nearly 200 villages having banned the sale of tobacco. De-addiction clinics have been set up, and schools and teachers are learning about the ill effects of tobacco. Intermediate results have been positive, though we will only know if this pilot is successful when it concludes in August 2019.
Muktipath seems to be the first example—in India, and possibly, the world–of an integrated approach to tackle both issues simultaneously. We are hopeful that the results will hold important lessons for public health, and for development efforts, in the future.